Weidan Cao
Assistant Professor, Department of Biomedical Informatics, The Ohio State University College of Medicine

Department of Biomedical Informatics
The Ohio State University
Email: weidan.cao@osumc.edu
Background
Dr. Weidan Cao is an Assistant Professor in the Department of Biomedical Informatics at The Ohio State University College of Medicine. She leads The Ohio State University Human-Centered Artificial Intelligence (OSU HAI) Lab. Dr. Cao’s research focuses on AI-empowered remote patient monitoring, AI-enabled clinical decision support system development and evaluation, mHealth apps/intervention engagement, the intended effects and unintended effects of mHealth apps/interventions, the usability and usefulness of mHealth apps for chronic disease management (e.g., cardiovascular diseases, cancer), patient engagement, doctor-patient communication, and cultural factors in health interventions.
Education and Training
- Postdoctoral Fellow, Biomedical Informatics, The Ohio State University, 2022
- PhD, Health Communication, Temple University, 2017
News
| Oct 01, 2025 | We currently have openings for PhD students and Postdoctoral associates in human-computer interaction and healthcare informatics. If you are interested in joining our team, please send me an email. |
|---|
Selected publications
-
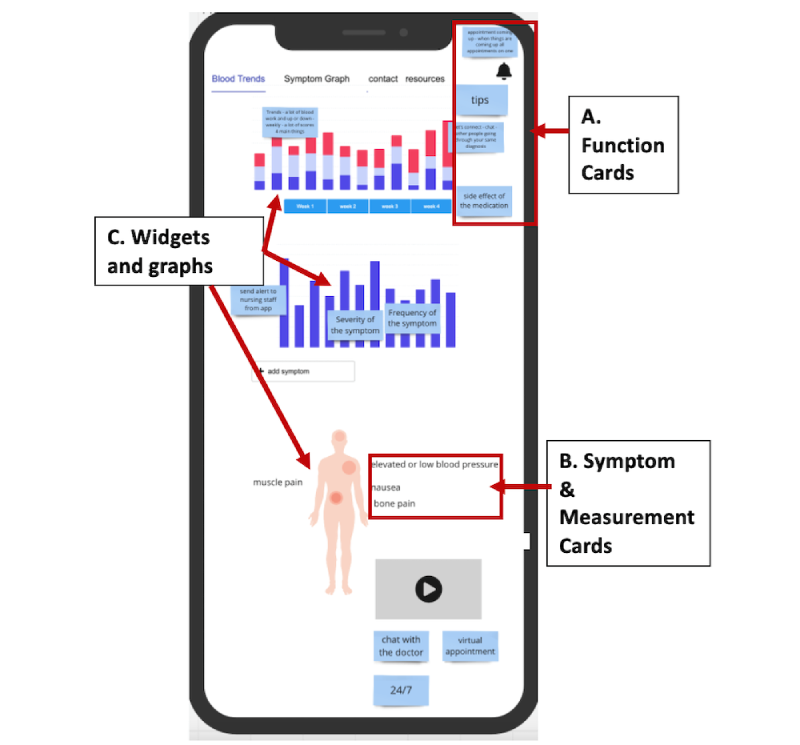
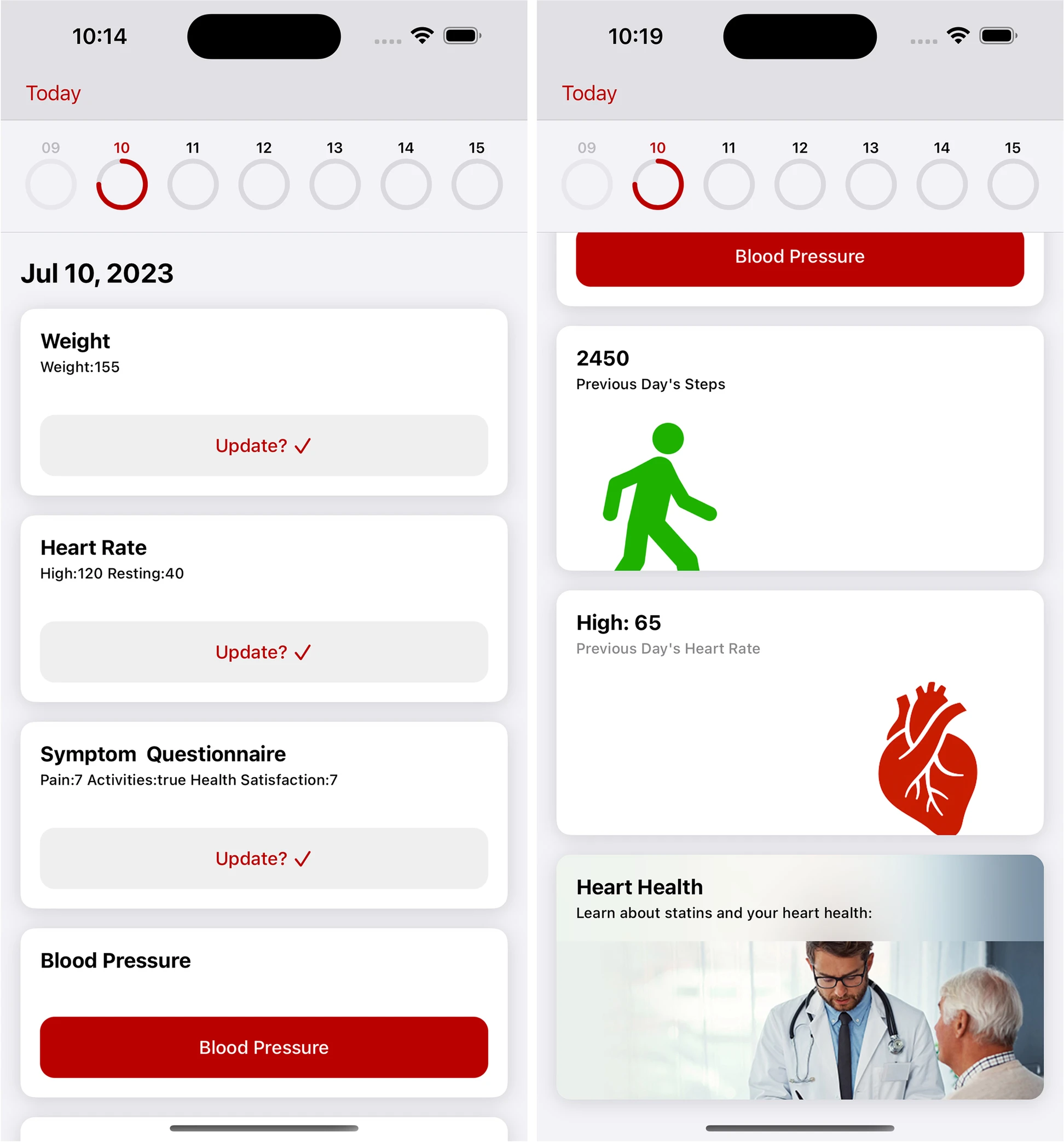
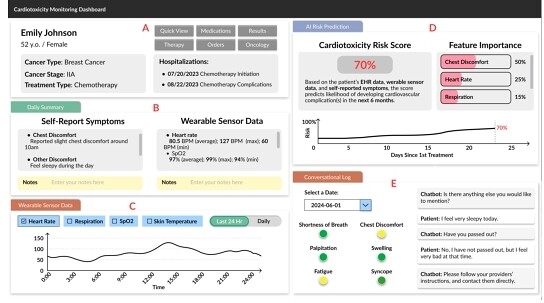 CardioAI: A Multimodal AI-based System to Support Symptom Monitoring and Risk Prediction of Cancer Treatment-Induced CardiotoxicityIn Proceedings of the 2025 CHI Conference on Human Factors in Computing Systems, Yokohama Japan, 2025
CardioAI: A Multimodal AI-based System to Support Symptom Monitoring and Risk Prediction of Cancer Treatment-Induced CardiotoxicityIn Proceedings of the 2025 CHI Conference on Human Factors in Computing Systems, Yokohama Japan, 2025